In recent years, the concept of painless deaths has gained significant attention worldwide. It is a topic that intersects medical science, ethics, and legal frameworks, making it both complex and thought-provoking. Painless deaths refer to the process of ending one's life without experiencing pain, often through medical assistance or specific techniques.
As society evolves, the conversation around end-of-life care and autonomy has become more open. People are increasingly seeking ways to ensure dignity and comfort during the final stages of life. This has led to debates about the legalization and regulation of practices that allow for painless deaths.
This article aims to explore the various aspects of painless deaths, including the methods, ethical considerations, legal implications, and societal perspectives. By the end of this article, readers will have a comprehensive understanding of the topic and its significance in modern healthcare.
Table of Contents
- The Concept of Painless Deaths
- Methods of Achieving Painless Deaths
- Ethical Considerations
- Legal Frameworks Around the World
- The Role of Medical Professionals
- Psychological Implications for Patients and Families
- Religious Perspectives on Painless Deaths
- Global Statistics and Trends
- Alternatives to Painless Deaths
- The Future of End-of-Life Care
The Concept of Painless Deaths
Painless deaths represent a significant shift in how society approaches end-of-life care. Traditionally, death was often accompanied by suffering, but advancements in medical science have made it possible to alleviate pain and discomfort. The concept revolves around providing individuals with the option to choose how they wish to depart this world, ensuring that the process is as humane and respectful as possible.
Medical professionals play a crucial role in facilitating painless deaths. They are trained to administer treatments and medications that can induce a peaceful transition. This includes the use of sedatives, analgesics, and other palliative care measures. However, the implementation of these practices varies across different regions, depending on local laws and cultural norms.
It is essential to understand that painless deaths are not synonymous with euthanasia or assisted suicide. While these terms are often used interchangeably, they refer to distinct processes. Euthanasia involves a physician administering a lethal dose of medication, whereas assisted suicide involves the patient taking the medication themselves. Both practices aim to achieve a painless death but differ in execution.
Defining the Process
To better comprehend painless deaths, it is necessary to break down the process into its core components:
- Preparation: This involves discussing the patient's wishes with family members and healthcare providers.
- Administration: The appropriate medications are administered under strict medical supervision.
- Monitoring: The patient's condition is closely monitored to ensure a smooth and painless transition.
Methods of Achieving Painless Deaths
There are several methods used to achieve painless deaths, each with its own set of advantages and limitations. The choice of method depends on various factors, including the patient's medical condition, personal preferences, and legal regulations.
One of the most common methods is the use of palliative sedation. This involves administering sedatives to induce a state of unconsciousness, allowing the patient to pass away peacefully. Another method is the administration of barbiturates, which are powerful sedatives that can induce a deep sleep from which the patient does not awaken.
In some cases, patients may opt for dehydration and starvation, a controversial method that involves withholding food and water. While this method is legal in many jurisdictions, it raises ethical concerns and is not universally accepted.
Medical Methods and Their Effectiveness
Medical professionals rely on a variety of techniques to ensure painless deaths. These methods are backed by scientific research and are continuously refined to improve patient outcomes. Some of the most effective methods include:
- Palliative Care: Focuses on relieving pain and managing symptoms.
- Terminal Sedation: Involves the use of sedatives to induce a peaceful state.
- Voluntary Stopping of Eating and Drinking (VSED): A patient's choice to cease food and water intake.
Ethical Considerations
The ethics surrounding painless deaths are complex and multifaceted. On one hand, proponents argue that individuals have the right to choose how they wish to die, especially if they are suffering from terminal illnesses. On the other hand, opponents raise concerns about the potential for abuse and the slippery slope that such practices could lead to.
One of the primary ethical dilemmas is the concept of autonomy versus vulnerability. While patients have the right to make decisions about their own bodies, there is a risk that vulnerable individuals, such as those with mental health issues, may be coerced into making irreversible choices.
Additionally, the involvement of medical professionals in facilitating painless deaths raises questions about the role of doctors in preserving life versus assisting in death. This tension is further complicated by cultural and religious beliefs that may conflict with the practice.
Addressing Ethical Challenges
To address these challenges, it is essential to establish clear guidelines and safeguards. This includes:
- Psychological Evaluation: Ensuring that patients are making informed decisions without coercion.
- Legal Oversight: Implementing regulations to prevent abuse and protect vulnerable individuals.
- Education and Awareness: Promoting understanding of the practice among healthcare providers and the general public.
Legal Frameworks Around the World
The legality of painless deaths varies significantly across different countries and regions. In some places, such as the Netherlands and Belgium, euthanasia and assisted suicide are fully legalized and regulated. In others, these practices remain illegal, with strict penalties for those who violate the law.
For example, in the United States, the legality of assisted suicide depends on the state. Oregon was the first state to legalize the practice through the Death with Dignity Act, which allows terminally ill patients to request medication to end their lives. Since then, several other states have followed suit, including Washington, Vermont, and California.
In contrast, countries like India and China have strict laws against assisted suicide, with penalties ranging from imprisonment to fines. These legal differences reflect the diverse cultural and religious values that shape societal attitudes towards painless deaths.
Comparative Legal Analysis
A comparative analysis of legal frameworks reveals the following key points:
- Europe: Countries like Switzerland and Luxembourg have progressive laws regarding painless deaths.
- Australia: The state of Victoria legalized voluntary assisted dying in 2019, joining other regions in adopting similar legislation.
- Asia: Countries like Japan and South Korea are still grappling with the issue, with ongoing debates about legalization.
The Role of Medical Professionals
Medical professionals are at the forefront of the painless deaths movement. They are responsible for ensuring that patients receive the highest standard of care during the end-of-life process. This involves not only administering medications but also providing emotional support to patients and their families.
Doctors and nurses undergo specialized training to prepare them for the unique challenges of end-of-life care. This includes understanding the legal and ethical implications of their actions and maintaining open communication with patients and their loved ones.
Furthermore, medical professionals play a crucial role in advocating for policy changes that promote compassionate care. By sharing their experiences and expertise, they can influence lawmakers to create more supportive environments for patients seeking painless deaths.
Challenges Faced by Healthcare Providers
Despite their best efforts, healthcare providers face numerous challenges when facilitating painless deaths. These challenges include:
- Moral Distress: The emotional toll of participating in practices that conflict with personal beliefs.
- Legal Risks: The potential for legal repercussions in jurisdictions where practices are not fully legalized.
- Public Perception: Navigating societal attitudes that may be hostile towards the practice.
Psychological Implications for Patients and Families
The psychological impact of painless deaths extends beyond the patient to their families and loved ones. For patients, the decision to pursue a painless death can be both empowering and daunting. It requires them to confront their mortality and make difficult choices about their future.
Families, on the other hand, may experience a range of emotions, from relief to guilt. Some may feel comforted knowing that their loved one is no longer suffering, while others may struggle with feelings of loss and regret. Counseling and support groups can play a vital role in helping families navigate these emotions.
It is important to recognize that the psychological implications of painless deaths are deeply personal and vary from individual to individual. What may be a source of comfort for one person may be a source of distress for another.
Support Systems for Families
To address these implications, it is essential to establish robust support systems for families. These systems can include:
- Counseling Services: Providing professional support to help families process their emotions.
- Support Groups: Creating spaces for families to share their experiences and connect with others.
- Education Programs: Offering resources to help families understand the process and its implications.
Religious Perspectives on Painless Deaths
Religion plays a significant role in shaping societal attitudes towards painless deaths. Different faiths have varying views on the sanctity of life and the morality of assisted suicide. For example, many Christian denominations oppose the practice, arguing that life is a gift from God that should not be terminated prematurely.
In contrast, some Buddhist and Hindu traditions emphasize the importance of compassion and may view painless deaths as an act of mercy. These differing perspectives highlight the complexity of the issue and the need for respectful dialogue between people of different faiths.
It is important to approach these discussions with sensitivity and an open mind, recognizing that religious beliefs are deeply personal and should be respected.
Interfaith Dialogue
Promoting interfaith dialogue can help bridge the gap between differing perspectives. This involves:
- Facilitating Discussions: Creating platforms for people of different faiths to share their views.
- Encouraging Empathy: Helping individuals understand and appreciate the beliefs of others.
- Promoting Compassion: Fostering a culture of kindness and understanding in end-of-life care.
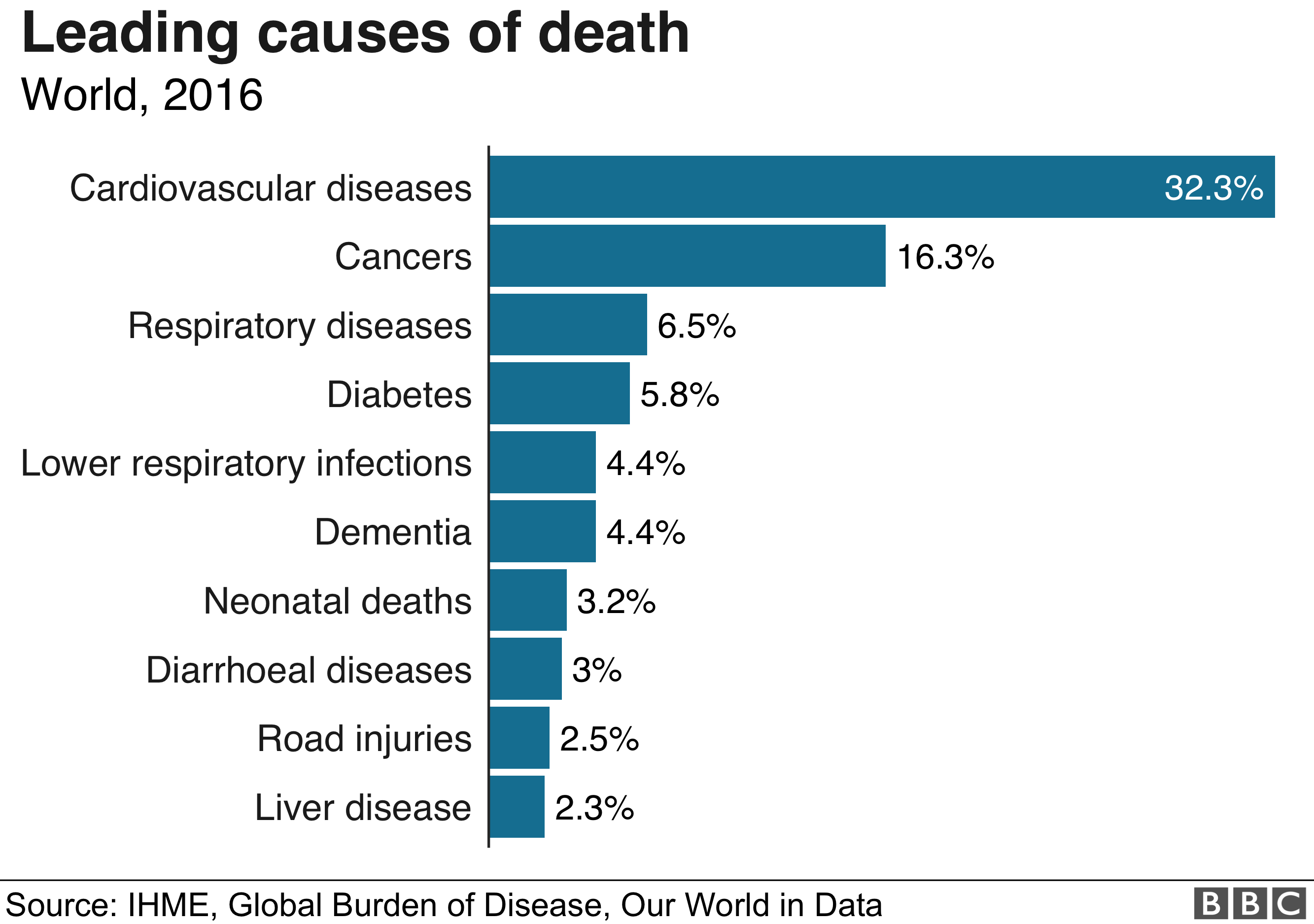
Global Statistics and Trends
Data from around the world provides valuable insights into the prevalence and acceptance of painless deaths. According to a study published in the Journal of Medical Ethics, the number of people opting for euthanasia and assisted suicide has been steadily increasing in countries where these practices are legal.
In the Netherlands, for example, the rate of euthanasia has risen from 1.7% of all deaths in 2001 to 4.5% in 2019. Similarly, in Oregon, the number of people utilizing the Death with Dignity Act has increased from 38 in 1998 to 245 in 2020.
These trends suggest that as society becomes more accepting of painless deaths, more people are choosing this option as a way to ensure a dignified end-of-life experience.
Interpreting the Data
When interpreting these statistics, it is important to consider the following factors:
- Cultural Context: Understanding the cultural and societal norms that influence decision-making.
- Legal Frameworks: Recognizing the impact of legal regulations on the availability of painless deaths.
- Public Awareness: Acknowledging the role of education and awareness campaigns in shaping attitudes.
Alternatives to Painless Deaths
While painless deaths offer one solution to end-of-life care, there are alternative approaches that focus on improving quality of life rather than hastening death. These alternatives include:
- Hospice Care: Providing comprehensive support to terminally ill patients and their families.
- Palliative Care: Managing pain and symptoms to enhance comfort and well-being